
Autoimmune diseases arise because the adaptive immune defense believes that an organ in the body is suddenly an enemy that must be combated.
The adaptive immune defense, also called the specific immune defense, is the part of the immune defense that is an acquired system and functions as a complement to the inborn immune defense. It consists of two kinds of lymphocytes, T and B cells. The T cells identify pathogenic substances, so-called antigens, such as bacteria or viruses.
An immunological memory is developed when T cells with specific receptors for the substance the body is exposed to grow in number. B cells also multiply and produce antibodies against the substance. In this way, a defense reaction starts, an immune response, in infections or vaccinations. In autoimmunity, something goes wrong. There are then both T cells with specific surface receptors and B cell-producing antibodies targeting components in the body itself. In MS, they target components in the central nervous system and in rheumatoid arthritis components in joints.
Development of MS
When MS is developed, autoimmunity occurs when certain lymphocytes make their way past the brain-blood barrier, which functions as a protective filter between the blood circulation and the brain.
These lymphocytes have key receptors that target, and recognize, components in the nervous system. Upon this recognition, the cells are further activated and release signal substances that attract more white corpuscles, which increase the inflammation, causing inflammatory damage. The covering surrounding the nerve cells is damaged, which disrupts or cuts off the signal paths for the nerve impulses that are supposed to go through. This can cause visual disturbances or a loss of touch perception in people with MS. In people with rheumatoid arthritis, the cartilage in joints is attacked in a similar way.
“In the project we are putting a lot of effort into studying the adaptive immune defense. We want to understand the key molecules on the T cells and what key antigens they bind to in joint cartilage, the central nervous system, and muscles,” says Tomas Olsson, professor of neurology at Karolinska Institutet.
Complex interaction
The HLA gene complex has been shown to play a major role in the development of autoimmune diseases, even though the gene is often not sufficient in itself. Other genes, lifestyle, and environmental factors are also involved. Today researchers can produce HLA molecules in their laboratories, which is a major step forward.
“We can, for instance, arm them with target antigens that seek out T cells, so we understand which ones they are. With the help of this knowledge, we can try to develop immune-specific treatments in laboratory animals,” explains Tomas Olsson.
Besides the HLA gene there are more than a thousand other genes that are involved in various immune reactions. When it comes to MS, there are some one hundred involved.
The central part in activating an adaptive immunity is the T cell’s receptor that binds to the HLA molecule, which in turn has bound a peptide to itself. In other words, there are three components involved: the T cell receptor, a peptide, and an HLA molecule. This is often called the trimolecular complex. If it is a virus peptide, this is good, because the virus will then be combated, but if the peptide instead comes from, or is similar to, parts of the central nervous system or joint cartilage, it attacks the tissue it is supposed to defend, which starts a pathogenic autoimmune process.
Paves way for new treatment method
The structure of the HLA molecule, which in turn determines which peptides can bind to it, varies greatly among individuals and is hereditary. For MS the HLA molecule variant that increases the disease risk is considerably more common in Nordic populations compared with people from the south. In Sweden 30 percent of the population carry the risk-elevating HLA gene variant.
“Part of the project is about understanding the interaction and which peptides are recognized by the HLA molecule. The idea is that HLA molecules provide the preconditions for different bindings of peptides that affect the brain and cause MS or affect cartilage and cause rheumatoid arthritis.”
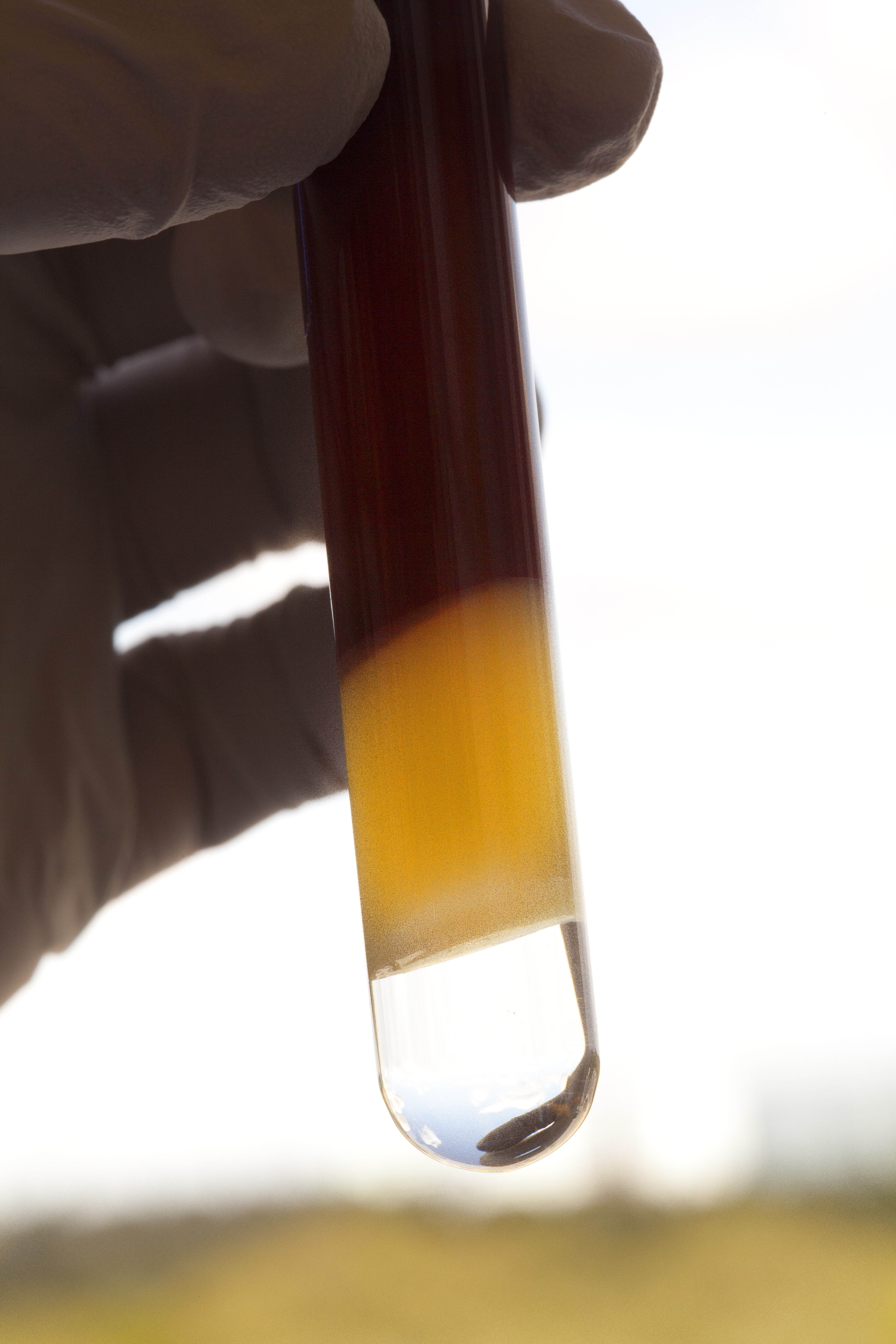
The hope is that it will be possible in the future via blood, spinal fluid, and joints to recognize the pathogenic cells and their function.
“It may be possible to use peptides to cure autoimmune diseases using principles similar to those behind hyposensitivity treatment of allergies, which are also unwanted immune reactions,” Olsson speculates.
Smoking a major risk factor
The reason smoking, together with certain HLA gene variants, dramatically increases the risk of MS and rheumatoid arthritis is thought to be irritation of the airways, which leads to increased inflammation. The inflammation can also activate or bring with it autoimmune cells. Smoke can also change peptides, making them more immune inducing.
“This is why we also have competence in respiratory medicine onboard in the project. We want to isolate cells in lung fluid to see if there are HLA molecules that have bound relevant peptides as autoantigens in MS and RA,” explains Tomas Olsson.
He also says that the project is a high-risk project and offers no guarantees that they will attain a complete understanding that leads to a cure.
“But no matter what we will be generating important new knowledge about genes and these diseases,” Tomas Olsson promises.
Text Carina Dahlberg/KAW
Translation Donald S. MacQueen
Photograph Magnus Bergström