The mucosa of the body – in our lungs and intestines for example – contain innate lymphoid cells. Jenny Mjösberg’s research team is studying these cells in tissue samples from people suffering from IBD – inflammatory bowel disease. One goal is to understand why some people respond better to biodrugs than others, and thereby make a contribution to precision medicine.
Jenny Mjösberg
Professor of tissue immunology
Wallenberg Academy Fellow, prolongation grant 2018
Institution:
Karolinska Institutet
Research field:
Innate lymphoid cells and their role in development of inflammatory bowel diseases and bowel cancer
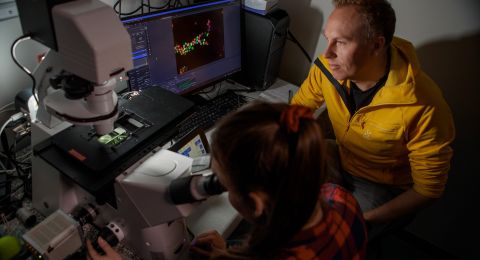
The type of cell that Mjösberg is examining in the lab at Karolinska Institutet (KI) just south of Stockholm is found in our intestines and elsewhere. The cells are called innate lymphoid cells – ILCs – and form part of the first line of defense in our immune system. They appear to play a specific part in the occurrence of inflammations.
“We want to learn more about ILCs, and in particular, we are attempting to find out the processes involved in IBD. The type of in-depth analysis we have performed in our lab enables us to study individual cells, so we can identify the genes and molecules that are potential targets for treatment,” Mjösberg says.
She explains that inflammatory bowel diseases, such as ulcerative colitis and Crohn’s, often affect fairly young people. IBD sufferers also run a greater risk of developing colon cancer. Mjösberg is inspired by the prospect of being able to make a difference in the lives of people with these diseases, which cause much suffering and a lower life quality.
“But I think the research process itself is fantastic. The dynamic – being a research leader and supervising students, working in a team, and the fact that I have creative freedom.”
“The grant gives me continuity in my research and is an acknowledgement that I have achieved good results. It also enables me to continue working at the same tempo, without losing momentum, which means an awful lot.”
Thanks to progress in research on immune cells and immune system mechanisms, scientists are starting to gain a better understanding of why individuals respond differently to medical treatments. And Mjösberg’s research is also making a valuable contribution.
“The research we’re doing paves the way for precision medicine – therapies tailored to the individual.”
Useful lesson from tonsils
A few years ago Mjösberg collaborated successfully with Rickard Sandberg, also based at KI, in a study of ILCs in tonsils using a technique for single-cell RNA sequencing. Their work generated many new ideas. She elaborates:
“It was the first time we’d been able to obtain such a detailed insight into processes in these cells. Our findings were really useful to many other researchers in the field. The project also gave us a whole list of biomarkers that we could use in our further studies. We’d never have known what to look for if we hadn’t sequenced the RNA of tonsil cells.”
So far, Mjösberg’s research team has used the findings in studies into type 2 inflammation, such as asthma and allergies, along with IBD and colorectal cancer.
“You might say we have described the new mechanisms by which ILCs contribute to these four pathological states, and the mechanisms that are targets for treatment.”
Clinical collaboration
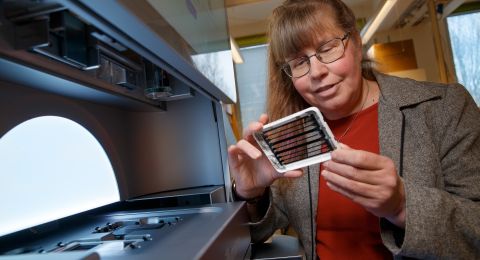
As a Wallenberg Academy Fellow, Mjösberg is continuing to map the intestinal immune system in the context of inflammation. The team is working closely with the gastroenterological and colorectal surgery departments at Karolinska University Hospital. This gives them access to fresh tissue samples from patients suffering from inflammatory diseases and colon cancer.
The research team is also collecting biopsies and blood samples from patients being treated with biodrugs. There are several such treatments for IBD. This work is taking place in close cooperation with three hospitals in Stockholm.
“This is where the precision medicine dimension comes in. We’re monitoring patients over time to see developments before and after treatment. It would be fantastic if we could arrive at something of value in this respect.”
We now know that our immune system is highly specific, and adapted to the tissue in which it is present. So not only do we have a very large proportion of the immune system in our intestines; it is also specialized to protect intestinal function. Mjösberg explains:
“Understanding healthy mechanisms is just as important as understanding inflammatory processes. Current biodrugs often work by blocking or knocking out a molecule driving the inflammation. But it’s also conceivable that we could strengthen molecules that protect or help tissue to heal, for example.”
Rapid pandemic initiative
Mjösberg’s team is part of the Center for Infectious Medicine (CIM) at Karolinska Institutet. When the coronavirus pandemic reached Sweden in spring 2020, CIM quickly became involved in research into Covid-19. Funded by Knut and Alice Wallenberg Foundation, the research teams jointly produced an atlas of the immune system for ICU patients with severe Covid-19.
“All data were made available to other researchers. My team was responsible for a small part of the atlas. We worked intensively on it for two months, before resuming our own research. We have seen how important it is to have basic funding for research. If the quality of research is high, researchers can be deployed in this way as needed.”
Text Susanne Rosén
Translation Maxwell Arding
Photo Whitney Weigel