Project Grant 2018
Translating mechanisms of cytotoxicity in natural killer cells and gamma-delta T cells into next generation cell-based cancer immunotherapy
Principal investigator:
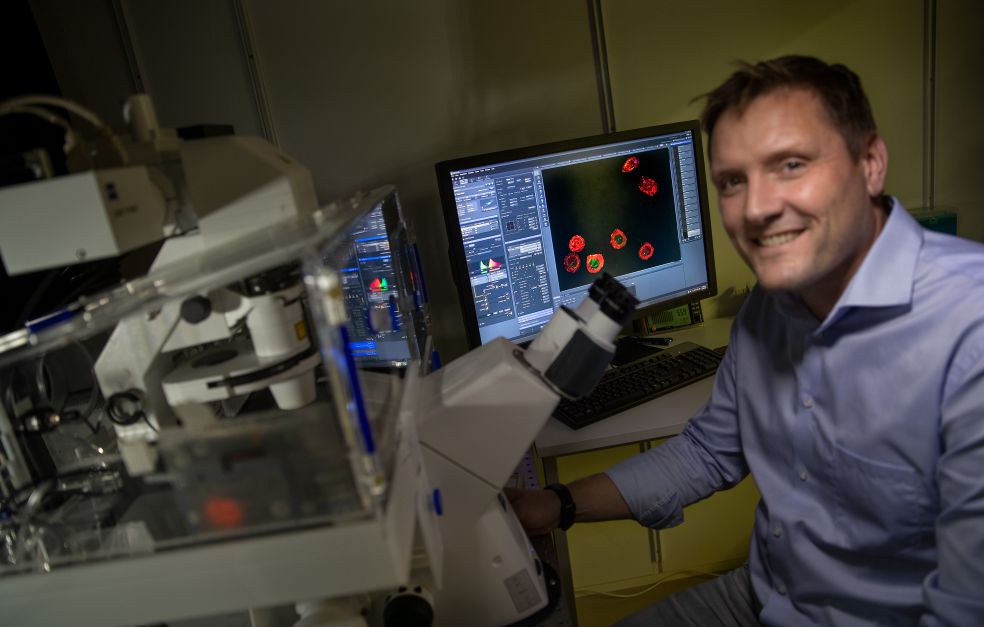
Professor Björn Önfelt
Co-investigators:
KTH Royal Institute of Technology
Professor Martin Viklund
Karolinska Institutet
Karl-Johan Malmberg
Michael Uhlin
Institution:
KTH Royal Institute of Technology
Grant in SEK:
SEK 31.2 million over five years
Immunotherapy offers promise in the treatment of cancer, particularly leukemia. But many questions remain to be answered before treatment can be as effective as possible. Those answers are to be found at cell level.
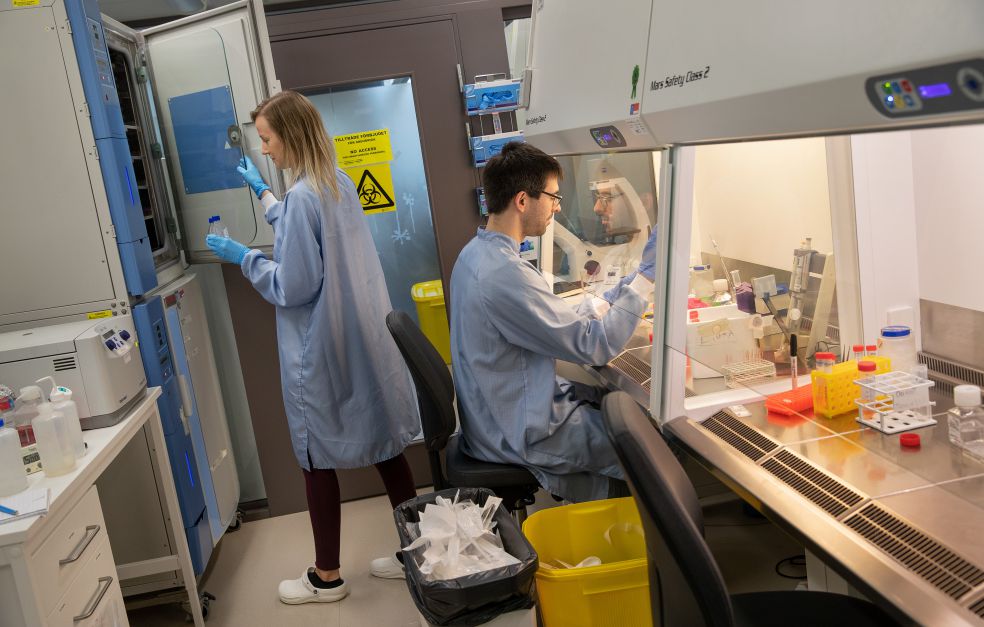
Immunotherapy uses the body’s own defenses. Our immune system contains white blood cells that are able to identify and kill tumor cells. Researchers want to be clear about how immune cells detect and break down tumor cells.
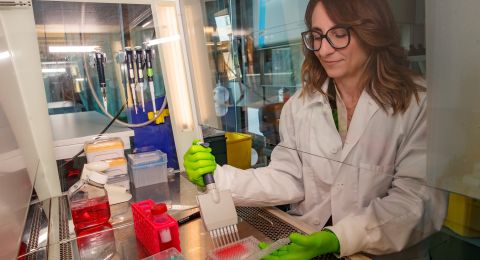
A research team at KTH Royal Institute of Technology and Karolinska Institutet has created a unique technical platform to study these “killer cells”. Björn Önfelt is a professor of biophysics, and is heading the multidisciplinary project.
“Our recipe for success is to operate at the interface between physics and immunology,” he explains.
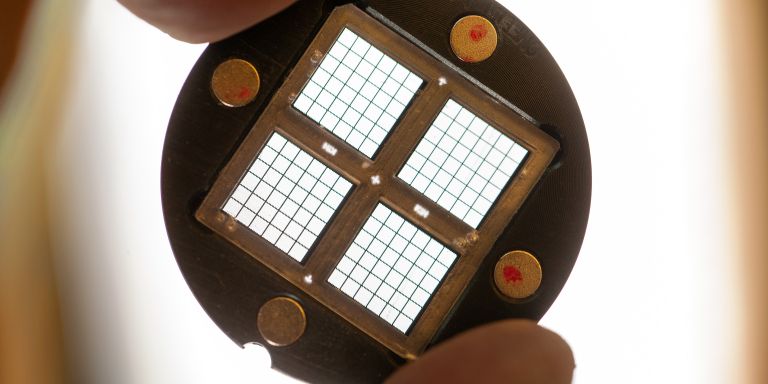
Cell close-ups on a microchip
The technical platform consists of various microchip-based methods. One involves a miniature version of the classic microplate used in biomedical research. The microchip contains up to 30,000 sample wells packed into an area not much larger than a thumbnail. The researchers bring together a certain number of tumor cells with killer cells in each well, and can observe the behavior and function of individual cells.
“The beauty of this method is that we can monitor individual cells for long periods. We obtain detailed information about individual cells, along with data on the cell population as a whole.”
The research is focusing on two types of killer cells: NK (natural killer) cells and T cells. The cells behave in different ways. Some are inactive; others are highly mobile, and are able to kill multiple cancer cells in a short time.
“Our experiments have shown us that there is often a group of cells that are really good at killing tumor cells, and we are naturally interested in knowing more about those cells, and why they are so effective,” Önfelt says.
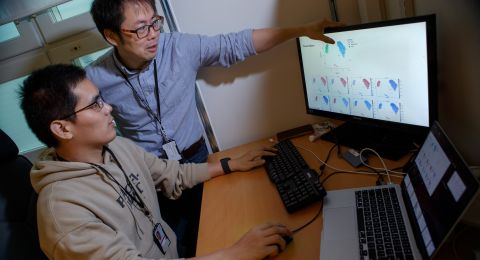
The whole picture
One central task is to characterize cell properties. The aim is to obtain as complete a picture as possible. This entails combining studies of cell biochemistry with analyses of their function.
“There are a fair number of molecules inside and on the surface of the tumors and the immune cells that regulate cell biological processes – we still don’t know enough about them,” Önfelt explains.
Detailed information about these processes may enable researchers to devise ways of manipulating entire cell populations to make them more effective. But it may be difficult to figure out all the interrelationships that are involved. The cells that seem to be best on paper are not necessarily the ones that are most effective in the long term, i.e. those able to survive in a patient and retain their ability to kill tumor cells.
“There may be desirable functions that we haven’t got to grips with yet.”
There is a sub-group of T cells that displays potential promise. These are called gamma-delta T cells, and share many properties with NK cells. As yet, too little is known about the biology of these T cells to make use of their full capacity, but they possess many attractive qualities. Since it is complicated to produce specific cells that match between donor and patient, many researchers consider the ideal would be a cell that suits everyone.
“A universal cell would be a gold mine, and this type of cell is a promising candidate,” says Önfelt.
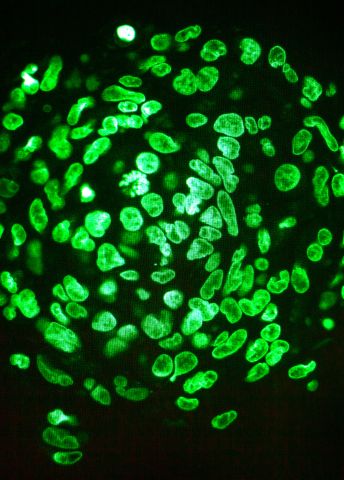
3D microtumors
A complementary method is to synthesize microtumors in 3D. The method combines a microchip with an ultrasonic emitter. The ultrasound makes the chip vibrate at a predetermined frequency.
“If the size of the wells on the chip matches the frequency, a standing sound wave is created, leading the cells into the center of the well. If the cells are of the right type, they start to grow in a clump instead of a monolayer. This enables us to synthesize microtumors, which we can then use as a model system for solid tumors.”
The killer cells react in a different way in a three-dimensional environment than they do on a flat surface, and there are differences between the molecules expressed on the cell surface. Önfelt demonstrates this by playing a clip showing a tumor embedded in collagen, and surrounded by killer cells.
“In the clip we can see how the NK cells move on a timescale of 24 to 48 hours, and we see how the tumor gradually disintegrates.”
A project grant from Knut och Alice Wallenberg Foundation is enabling the researchers to improve and further develop the technical platform.
“Our entire research is making a quantum leap. We can explore a number of fundamental questions, but also contribute by making a detailed characterization of cell products already being used therapeutically. An additional driver is that our research should benefit patients,” Önfelt concludes.
Text Nils Johan Tjärnlund
Translation Maxwell Arding
Photo Magnus Bergström