However, Per-Olof Berggren emphasizes that it is mainly as a research tool that this method will have a crucial importance.
“Transplantation of the islets of Langerhans to the eye makes it possible to study the insulin-producing beta cells with a high resolution, over an extended period of time in the living organism with both intact vascular and nerve supplies. The eye functions as a natural window on the body,” confirms Berggren.
It sounds like a somewhat crazy idea, moving the pancreas' insulin-producing cells to the eye, but animal experiments have shown that it works and the step to testing the method on people is probably just a few years in the future.
“The studies we have done on monkeys in Miami indicate better blood sugar levels so we are very hopeful that it will also work on humans,” explains Per-Olof Berggren.
Gentler experimental method
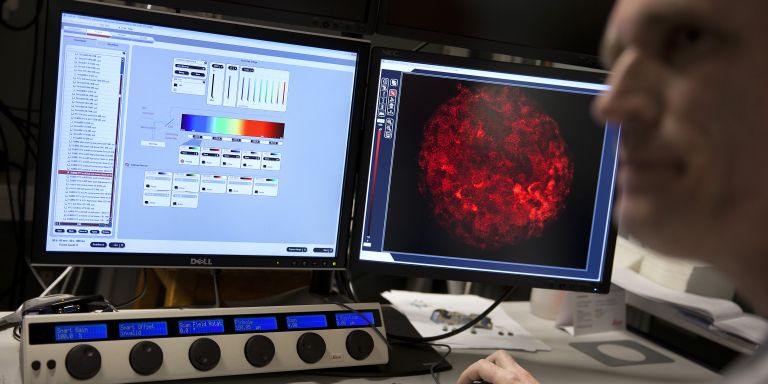
Using various kinds of advanced microscope systems, the researchers can follow the complicated process that regulates the release of insulin in real time.
“We obtain the entire system biology picture of what happens, without harming or killing the animals.”

As a Wallenberg Scholar, Berggren will take the experiments further. He has strong hopes over the next few years of clarifying in detail the processes that regulate the insulin release under normal conditions and why these do not work in diabetes in mice, monkeys and humans. This is of crucial importance to creating new and more adequate treatment principles for diabetes.
Rapidly growing widespread disease
Per-Olof Berggren is Professor of Experimental Endocrinology and director of the Rolf Luft Research Center for Diabetes and Endocrinology at Karolinska Institutet. He leads a research team of around 35 people in Stockholm, has intensive collaboration with researchers in Miami and Korea and is now building up further collaboration with researchers in Singapore. The goal is to understand the causes of one of the world's fastest growing widespread diseases - diabetes.
The fact that Korea and Singapore are cooperative partners is no happenstance. More than 11% of these countries' populations have diabetes, which is more than twice as many as in Sweden.
“Our collaboration is based on the research that takes place at Karolinska Institutet. The collaboration with Miami provides us high-quality human tissue while the experiments on monkeys are done in Asia,” he explains.
Important puzzle pieces
Berggren and his colleagues have focused on understanding the mechanisms behind the release of insulin. They want to map the signaling systems that are in the insulin-producing beta cells in the pancreas' islets of Langerhans. Besides the insulin-producing beta cells, the glucagon-producing alpha cells and somatostatin-producing delta cells are also involved in regulating the blood sugar levels. However, it is only the insulin that can lower the blood-sugar levels. In diabetes, the function of all three of these cell types is changed.
Berggren's research team has shown that the glucagon-producing alpha cells are stimulated by glucagon itself and that the same principle applies to the insulin-producing beta cells. This means that there is a self-regulating effect in the islet of Langerhans, where a cell that releases any of these hormones immediately gets an order to produce more of the released hormone.
“By obtaining knowledge of how the hormones regulate their own production, we can also study defects in the process on the long term. If the defects are of significance to diabetes, important puzzle pieces can fall into place,” says Per-Olof Berggren.

Difference between mice and men
A few years ago, the research team discovered that the structure of the islets of Langerhans, and consequently the regulation of insulin release, was different in humans compared with that in mice.
“It was an important discovery and we realized that the previous studies done on mice were not necessarily accurate with regard to humans.”
The islets of Langerhans in mice contain a large amount of nerves that have contact with the hormone-releasing cells. However, in humans, it turned out that the nervous system only has indirect contact with these cells by influencing the blood flow.
“This was unexpected. Nobody would have believed that the basal cellular mechanisms would differ so much between mice and men. The differences in function and structure are significant,” confirms Berggren.
The discovery that the release is not directly controlled by nerves, but rather indirectly by the nerves establishing contact with the capillaries in the islets of Langerhans can be of major importance to the development of future medicines against diabetes. However, the various hormone-releasing cells' location in the islets of Langerhans differs between mice, monkeys and humans. They are more mixed in both monkeys and humans.
Promising results
Around 90% of those who have diabetes, have type-2 diabetes, what we used to call adult-onset diabetes. Previously, it was only adults who became ill, but today children are also afflicted.
In type-2 diabetes, beta cells remain, but they are blind to changes in the blood-sugar concentration and do not release the right amount of insulin. In type-1 diabetes, which mainly afflicts children and adolescents, an autoimmune reaction occurs and the body's immune system kills the insulin cells.
“Together with researchers in Miami, we now use the eye as a platform for studying the various immunological and inflammatory reactions that take place in the islets of Langerhans in diabetes. We have already generated a number of exciting results in terms of the contact between beta cells and T cells and how this contact can be affected by, for example, applying various substances directly to the eye.”

Uncertain if the method works for people
After the successful experiments on curing diabetic mice, by transplanting islets of Langerhans to the anterior chamber of the eye, the research team has received many questions as to whether the method could also work on people and if it could replace the liver transplantations done today.
“It is impossible to say right now. What we can confirm is that the experiments we have done on diabetic monkeys in Miami have so far been very successful and are not associated with any problems for the animals at all. Even if we were unable to make the monkeys completely independent of insulin treatment, we were able to improve the blood-sugar regulation in that the transplanted beta cells began their own insulin production.”
One of the advantages of transplanting islets of Langerhans to the eye is that they are quickly supplied with blood.
“Even if enough islets of Langerhans cannot be transplanted to completely cure diabetes, the need for insulin injections can hopefully be reduced. It would be a major gain to be able to counteract harmful fluctuations in the blood-sugar concentration by increasing the diabetes patient's own insulin production,” confirms Per-Olof Berggren.
Text Carina Dahlberg
Translation Semantix
Photo Magnus Bergström