Why are more and more people suffering from allergies and autoimmune diseases? The answer may lie in the development of the immune system in newborns. Wallenberg Scholar Petter Brodin has developed a technique to map immune system development from a single drop of blood.
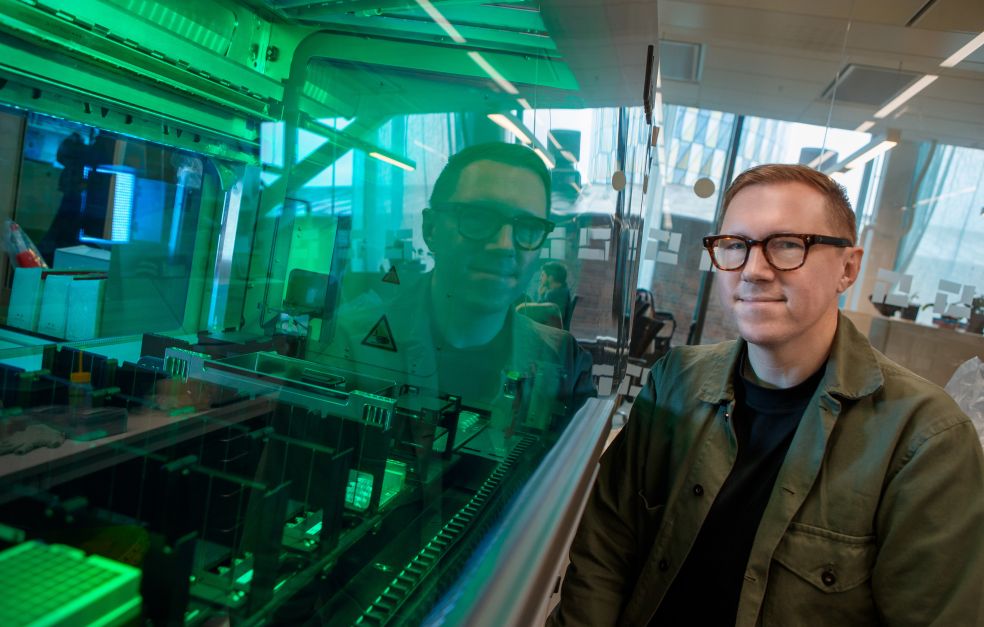
Petter Brodin
Professor of Pediatric Immunology and Pediatrician
Wallenberg Scholar
Institution:
Karolinska Institutet
Research field:
The early development of the immune system and why there are such large individual differences
Allergies, asthma and autoimmune diseases are much more common today than they were a century ago. No one knows exactly why, but theories abound. Brodin is seeking answers by charting immune system development from birth. He is studying blood and stool samples from delivery and on through childhood, hoping to find a solution.
“It used to be thought that children were somehow more vulnerable than adults. But a newborn baby’s immune system is highly efficacious. The difference is that it has no memory of earlier experiences.”
Our immune system is active 24/7, constantly searching for injuries and unwanted intruders such as bacteria and viruses. But it can only identify threats if it knows what is dangerous. Training of the immune system begins even before birth, when antibodies from the mother reach the unborn child via the placenta. After birth, the system develops dramatically, driven by encounters with bacteria, viruses and other microorganisms in the environment.
Brodin likens the immune system to a sixth sense that detects and adapts to everything we encounter daily.
“Infants soon begin putting almost everything they see into their mouths. This allows their immune system to sense the bacteria and particles in their environment and learn from them.”
Monitoring 500 children
He has spent many years refining the methods required to understand how this learning occurs. Today, his research team is a world leader in this field. To date they have collected blood and stool samples from over 500 children, whom they monitor until the age of four. New samples are regularly taken and analyzed at the Biomedicum research center in Solna. The team is studying immune cell activity in the blood and the composition of gut bacteria to learn more about the biological mechanisms that guide development.
One challenge has been to analyze the small amount of blood that can be taken from a newborn child. However, they have now developed a technique to track proteins as well as the 100 or so types of white blood cell contained in a single drop of blood.
As he shows us around the lab, Brodin points proudly to an analytical instrument several meters long that has been designed by his research team. Under the instrument’s black cover lies an automated platform that processes a tiny blood sample, breaking it down into even smaller parts for analysis. This analysis reveals the function of all the white blood cells present in a drop of blood.
“Human precision is nowhere near as exact as an automated platform. We can use it to do much more with smaller volumes while maintaining precision.”
This approach is called systems immunology. It uses large-scale analysis to provide a comprehensive picture of the balance in a child’s immune system. Earlier research often focused on parts of the system, but this is a more holistic approach.
It is strong teamwork that moves us forward, not research stars doing pirouettes in the corners.
“The advancements of recent years have enabled us to perform more advanced analyses, incorporating data from all components of the system. This is necessary to create the comprehensive understanding we need in order to know what is right and wrong.”
Giving all children a good start
The analysis compares children born naturally with those delivered by cesarean section, as well as those born prematurely or at full term. Other factors, such as whether the child was breastfed or given formula, are also monitored. The goal is to identify the common denominators that give a child an optimal start in life.
“We know that children who receive antibiotics in the first months of their life run a greater risk of developing a variety of immune-related diseases, including asthma, allergies and autoimmunity. It would be amazing if we could nudge those children back in the right direction.”
Much of our early knowledge about the immune system comes from studies on mice, but these have created many misconceptions about its development. For reliable results, laboratory animals live in highly controlled environments, far removed from the real world where children grow up.
“It’s quite clear that our immune system is shaped by our environment. That’s why we need to conduct our research among children living normal lives.”
The research team includes chemists, biologists, immunologists, physicians and even programmers. An interdisciplinary approach is essential to gain a complete picture.
“The best part of research is working with gifted, driven people who possess completely different skills but work together toward a common goal,” says Brodin.
During the week, he divides his time between the research lab and his work as a specialist pediatrician at Astrid Lindgren Children’s Hospital.
"It is incredibly rewarding to work as a pediatrician, something I would miss if I were to stop. Meeting patients gives me knowledge and extra motivation to understand what can go wrong as the immune system develops,” he says.
Text Magnus Trogen Pahlén
Translation Maxwell Arding
Photo Magnus Bergström