DNA analysis technology has undergone a revolution in recent years. These days it is simpler, faster and cheaper to make a genetic diagnosis. Basic research discoveries can now play a part in clinical medicine, benefiting patients enormously in the process. It is seen as a breakthrough for precision medicine.
Anna Wedell
Consultant and Professor of Medical Genetics
Wallenberg Clinical Scholar, prolongation grant 2021
Institution:
Karolinska Institutet
Research field:
Use of whole-genome sequencing and transcriptomics in combination with biochemical and clinical data to transform diagnostics and identify new disease genes in patients with inherited metabolic disorders.
Researchers have long dreamt of using comprehensive information obtained from the patient’s own DNA to achieve accurate diagnosis and tailored therapies. This vision is now becoming a reality. Researchers can make use of modern whole-genome sequencing to map most or all of the DNA of individual patients, and identify mutations that cause diseases.
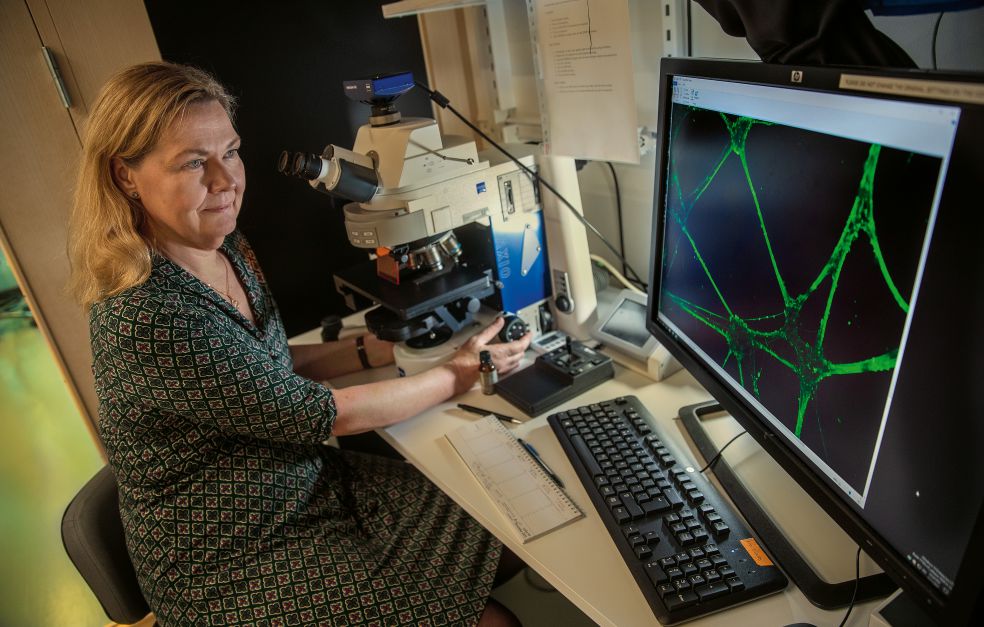
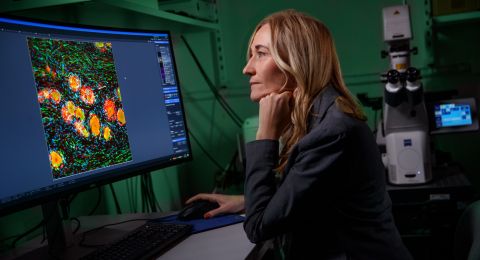
Anna Wedell is a consultant and professor of medical genetics at Karolinska Institutet, and a Wallenberg Clinical Scholar.
“It’s a huge leap forward to have access to the new methods. Before we could only study a few individual genes at a time. There has been a huge technological advance.”
The new methods offer particular potential for diagnosis of a diverse group of some 8,000 conditions, most of them inherited. Although each of these diseases is rare, taken together they affect many people.
“In Europe alone it is estimated that some thirty to forty million people suffer from one or more of these disorders,” says Wedell.
Dealing with these rare or completely unknown diseases poses a great challenge for the health care system. It often takes a long time for the patient to receive a diagnosis, and there may be a lack of knowledge about treatment or preventive measures. Targeted therapies currently exist for only five percent of all these rare disorders.
“But progress is now being made. We’re learning a great deal and we’re beginning to discern a completely new landscape of diseases.”
Research on congenital diseases
Wedell’s own research focuses on inherited metabolic diseases. Approximately one in two thousand children are born with an impaired metabolism, often leading to brain damage. These disorders are caused by inherited defects in the body’s biochemical reactions. Most organs may be affected, but the brain is particularly sensitive. Early treatment is therefore vital to prevent irreparable damage.
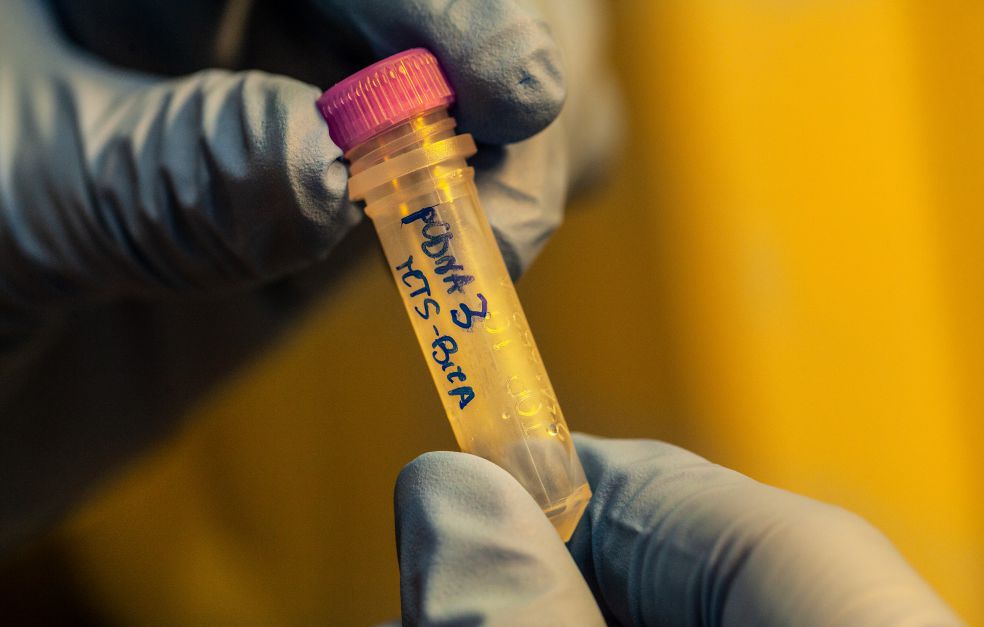
“Our patients often have unspecific symptoms and signs, making it difficult to establish the exact diagnosis. We make detailed clinical investigations of the patient and carry out sophisticated biochemical analyses combined with genomics. We also use various functional methods to validate new genetic variants that we find.”
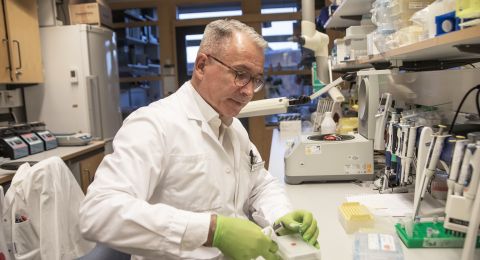
The researchers also take their findings into the basic research lab, creating models based on the patient’s cells or using model organisms. The models are used for in-depth experimental studies of disease mechanisms.
“Simply put, we want to discover new diseases, understand their underlying biology, and eventually attempt to treat them. The goal is to develop efficacious therapies.”
Collaboration opens the way for precision medicine
As a Wallenberg Clinical Scholar, Wedell has been working on a concept enabling new technology and basic research findings to be implemented in highly specialized medical care. This involves integrating genomics and bioinformatics with clinical expertise, which in turn requires new tools and new approaches. The initiative is taking place in close collaboration between SciLifeLab and Karolinska University Hospital, and has resulted in the Genomic Medicine Center at Karolinska – GMCK.
“It’s a new concept, establishing an interdisciplinary environment between academia and the health care sector. We want to join forces to address topics we have in common, instead of working in separate silos.”
Whole-genome sequencing of just over 3,000 patients was performed between 2015 and 2020. About 1,200 of them received a genetic diagnosis. The results are encouraging, and show that new groups of patients can be correctly diagnosed and also receive earlier treatment.
“This offers the prospect of radically improved diagnosis of rare disorders, ultimately saving lives. It’s a major leap forward for precision medicine.”
“The grant is absolutely crucial to our prospects of developing new approaches and creating a new collaborative culture. The funding has given me both authority and freedom to break new ground in a fairly conservative environment. Our work has also led to a new center for precision medicine that is intended to help bridge the gap between academia and the health care sector.”
Ground-breaking therapies
Wedell speaks of patients they have been able to help, like one girl, who had brain damage. A defective transporter was discovered, revealing a previously unknown link between different cell types in the brain, impacting the way white matter in the brain is formed.
“On the basis of that defect we could theoretically predict that a specific dietary therapy might help – one rich in fat.”
When the girl was put on a fat-rich diet her brain began to adapt and burn ketone bodies instead of carbohydrates.
“We could see how her white matter started to appear and her brain started to grow. It was an amazing experience. She won’t make a full recovery, however. With another patient we were able to act sooner, and in this case the prognosis is better.”
Research on diagnosis of rare disorders yields plentiful new knowledge. Some disease genes can be associated to other, more common diseases. Mapping the mechanisms underlying rare inherited disorders potentially opens the way for a better understanding of the metabolic components of more common diseases as well.
“Rare disorders yield knowledge of general relevance, knowledge that may ultimately lead to new treatment principles for other diseases,” Wedell says.
Text Nils Johan Tjärnlund
Translation Maxwell Arding
Photo Magnus Bergström