How does our immune system develop once we are born? What factors keep it on the right track? Wallenberg Academy Fellow Petter Brodin aims to study the process in detail. This has been made possible by radical new technologies and methods.
Petter Brodin
Associate Professor of Immunology, Pediatrician
Wallenberg Academy Fellow 2019
Institution:
Karolinska Institutet
Research field:
Early immune system development
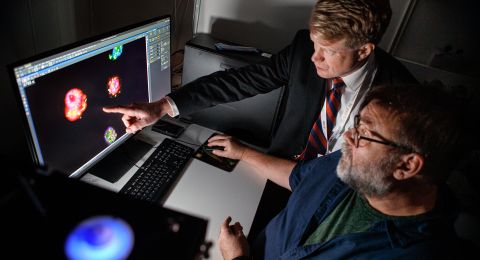
“We’re piecing together a developmental map of the infant immune system. This knowledge may improve our understanding of diseases caused by immune system reactions, such as allergies and autoimmune diseases,” Brodin explains.
Unique studies of new-born infants
When a child leaves the womb, its immune system develops rapidly. The changes result from exposure to bacteria, viruses and other microorganisms in the new surroundings.
It had long been difficult to study in detail what actually happens in a new-born infant. But in 2018 Brodin published a study involving 100 children, in which development in prematurely born infants was compared with that in those born on time.
“We were able to show that the immune system of infants born prematurely differed from that in children who had been born on time, but also that it adapts after a while. We now know that the immune system is highly dynamic early on in life,” Brodin says.
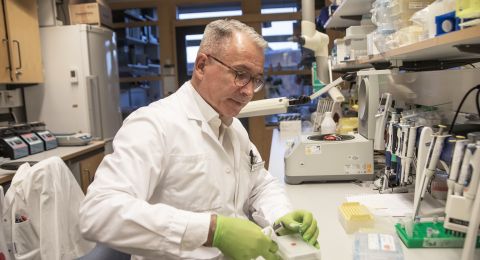
A blood sample from a new-born infant contains very little blood, which makes it hard to analyze. Additionally, it is difficult to establish the contact with infants and their parents that is needed to conduct the studies. One key factor has been that Brodin, and several other members of his team, divide their time between the research lab and clinical practice.
“When you do clinical work, you have a relationship with the children and their families, particularly in the case of premature babies, who spend their first weeks or months in hospital. We’ve been able to coordinate all collection of samples with the other care received by the children,” he says.
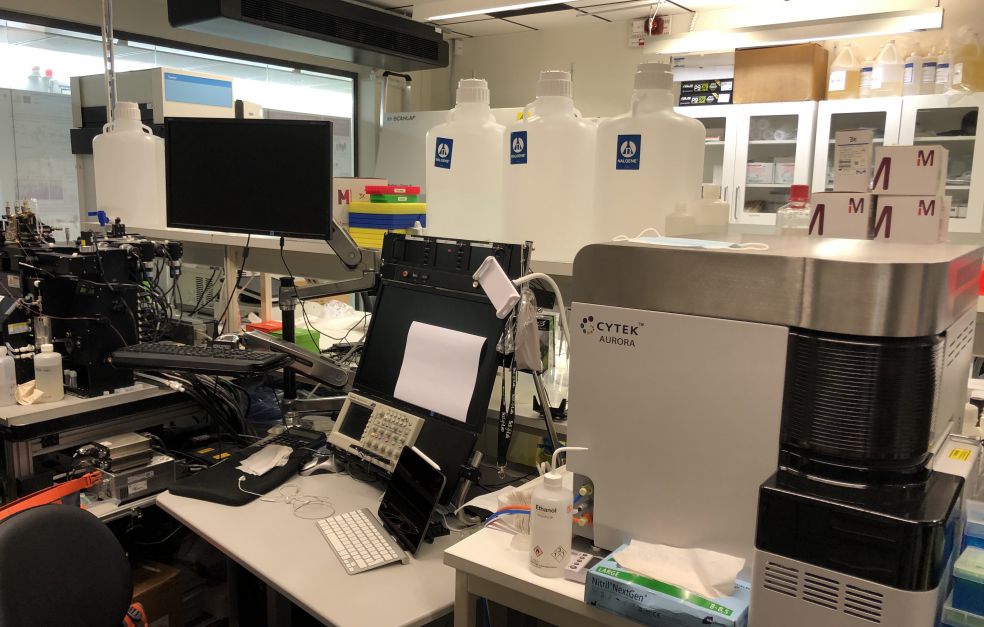
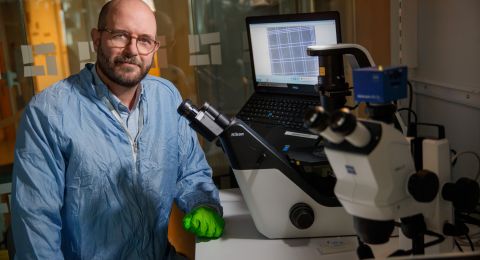
The research team has also developed new methods of managing and analyzing the minute samples. They are using techniques such as mass cytometry to count and identify all the white blood cells in a sample. That information can then be combined with extensive protein analyses.
By comparing samples from different points in time, the team gains an idea of how the child’s immune system is developing. To understand the complex process, they have collaborated with mathematicians in developing new software and algorithms.
“I’m proud of what we’ve achieved so far. Thanks to Knut och Alice Wallenberg Foundation, we can now pursue this globally unique project.”
“The Wallenberg Academy Fellow scheme enables me to carry out more analyses, more thoroughly, allowing me to make more progress in my research.”
The research team has also succeeded in showing which antibodies are passed on by the mother to the new-born child, and that there is no difference between the antibodies inherited by children born prematurely and those born on time.
“It’s an elegant evolutionary process whereby the mother’s immune system gives the new-born child initial protection, lasting a few months after birth.”
Monitoring 300 children
Some 300 children will be monitored up to the age of three, and blood and stool samples will be regularly taken from them. The results may yield a more thorough understanding of immune system development and factors affecting it.
“Among other things, there are specific bacteria in our gut microbiome that have developed in parallel with humans, and that are beneficial to us. We’re trying to find out if we can benefit from that knowledge so we can give children an optimal start in life.”
One long-term goal would be to take samples from all new-born infants to ascertain the status of their immune system. If there were any gaps in the system, it could be given a push in the right direction.
“That might enable us to prevent diseases related to early development of the immune system, such as autoimmune diseases and allergies. But first we have to identify optimum development,” he says.
Studies are also planned in other parts of the world. These may show whether infant development is the same everywhere or whether there are differences potentially due to environmental factors or genetic dissimilarities.
Driven by challenges
Brodin came late to medicine. As a boy he wanted to be a professional ice-hockey player or a musician. He enjoyed school, but seldom found it particularly stimulating.
“My parents were normal working people, and I never envisioned becoming a researcher. But when I was doing my military service, an officer spoke of higher education as a challenge. This whetted my appetite, since I’ve always been driven by challenges,” he explains.
He applied for and was offered a place on a medical research preparatory program, which introduced him to a variety of scientific fields. A meeting with Klas Kärre, an immunologist, had a decisive impact.
“After that I was hooked. Immunology is so extraordinarily complex – millions of cells communicating with each other, and working together to create a system that is incredibly powerful, yet perfectly balanced.”
During the pandemic he has shared his knowledge in the media and also participated in Covid-19 research. He is coordinating an international consortium that is gathering data on cases where people under the age of 50 without underlying conditions have been severely affected by the disease.
“The contacts I’m making in that context will contribute to our research into immune system development. The pandemic has been a catalyst for international collaboration, and has also shown how we researchers can focus when we have to.”
Text Magnus Trogen Pahlén
Translation Maxwell Arding
Bild Andreas Lundberg, Lakshmikanth Tadepally, Marcus Marcetic