About one-fifth of adults in Sweden live with chronic pain, which is often hard to diagnose and treat. Wallenberg Clinical Scholar Håkan Olausson has discovered a previously unknown type of pain-conducting nerve fiber. This may pave the way for new therapies.
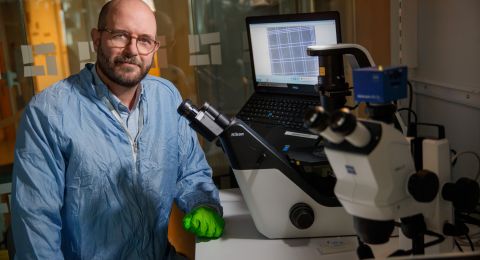
Håkan Olausson
Consultant and Professor of Clinical Neuroscience
Wallenberg Clinical Scholar 2020
Institution:
Linköping University
Research field:
High-speed pain signaling in humans
“It’s deeply unsatisfactory that so many people suffer from chronic pain. We discovered these fibers mostly by chance, and I hope they can help us to better understand how to treat pain,” Olausson says.
There are several kinds of nerve fibers in the body. They act as conduits for temperature, touch, pressure and pain. Although Olausson has worked a great deal with pain patients, most of his research concerns touch. He made the pain-related discovery when he and his colleagues were testing a measuring technique they had refined. Called microneurography, it involves inserting a thin needle into a single nerve fiber to measure the signals passing by. The technique has existed since the late 1960s, but has not been widely used, due to difficulties in inserting the needle correctly, a process that has sometimes taken hours. When Olausson’s research team used ultrasound to “see” the needle in the body, it took ten minutes to insert.
“When it became so much simpler, we were able to perform more experiments in a shorter time. On that particular occasion we wanted to examine a specific type of nerve fiber with receptors in the skin.”
The result was surprising. The receptor was found to require strong stimulation to be activated, but could also convey various degrees of stimulation. Both of these traits are characteristic of pain receptors. The remarkable aspect was that the signals were ultrafast, which had been thought to be impossible in humans. Ultrafast pain signaling systems had been found in other mammals, including apes and mice, but not in humans. The received wisdom put forward in all scientific literature on the nervous system had been that human pain impulses were conveyed by slow nerve fibers.
“As a Wallenberg Clinical Scholar I can recruit full-time clinical researchers. This gives our work an enormous boost.”
Unknown impact on the experience of pain
It now remains to find out what function the high-speed pain signals have. Olausson’s hypothesis is that they are essential so we can quickly move away from whatever is harming us. One of his PhD students has developed a method of measuring high-speed nerve signals when the back of the foot is subjected to painful stimulus.
“We’re well on the way to demonstrating that the system plays a key role in motor control and rapid evasion. But how does it impact our sensation of pain?”
Olausson wants to use magnetic resonance imaging (MRI) to find out. The camera reveals the parts of the brain where blood flow increases when the high-speed fibers are activated. The problem is that it is not possible to activate those nerve fibers alone without activating the slower ones. The solution is to block the signals by applying pressure to the nerves. Earlier research has shown that fast nerve fibers are always blocked first. There ought to be a later time window when only the slow nerve fibers are active. Early and late images can then be compared as a basis for conclusions as to which areas of the brain are activated by which fibers.
Olausson is conducting another experiment to ascertain whether the fibers and their receptors become more active in conjunction with inflammation. A third experiment entails examining patients with nerve damage due to chemotherapy – a very common problem in cancer treatment.
“This is a type of chronic pain. We want to see whether there is a link between the pain and the fast nervous system. In a way, we hope so. It would naturally make our discovery of the fibers all the more exciting because it would give us a new target for treatment of chronic pain. But although I’m enthusiastic as a researcher, we shouldn’t get ahead of ourselves by deciding in advance what we’re going to find. That’s when things can go wrong.”
Frustrated by the lack of help
Even as he studied medicine, Olausson was curious about research, having attended a lecture on temperature sensations in cats. He joined the lecturer’s research team, but became allergic to cats. He was obliged to move on to human feeling.
“In neurophysiological terms, the sense of touch, which has been one of my fields, is closely related to pain. But until now pain has been peripheral to my research. I was drawn to pain research by this unexpected discovery.”
As a doctor, he has met pain patients almost every day, and has often been frustrated by the lack of help available to them. It’s not uncommon that all a doctor can say is “everything seems fine”, which is not much consolation for a patient in pain.
Early in his career Olausson felt that working as a doctor gave a vital degree of stability as compared with the much more uncertain world of research. These days he thinks the two complement one another.
“There are highly skilled medical practitioners and gifted researchers, but it’s hard to find people who combine the two. Maybe I’d have been a better researcher or a better clinician if I’d stuck to one or the other. But I think my approach has yielded dividends.”
Text Lisa Kirsebom
Translation Maxwell Arding
Photo Charlotte Perhammar,Thor Balkhed Linköpings universitet