Project Grant 2013
Next generation of mucosal vaccines for protection against infectious diseases
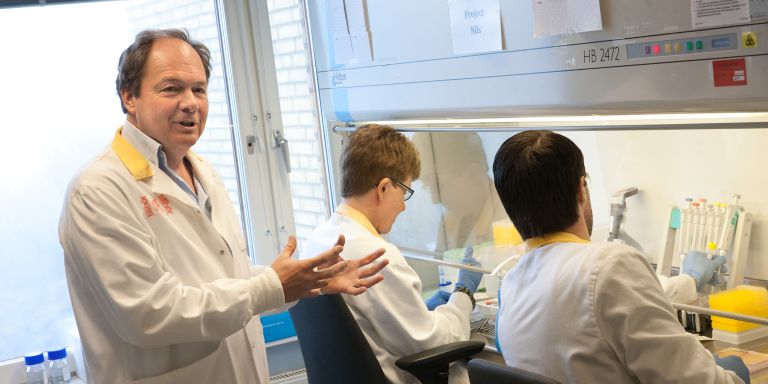
Principal investigator:
Nils Lycke, MD, PhD, Professor and consultant in Clinical Immunology
Co-investigators:
University of Gothenburg
Mary-Jo Wick
Chalmers University of Technology
Fredrik Höök
Marta Bally
Lund University
William Agace
Institution:
University of Gothenburg
Grant in SEK:
SEK 16.2 million over five years
To-date, nearly all vaccines are injected with a needle and syringe, but this has its disadvantages: repeated injections using the same syringes can transmit contaminating pathogens and cause infections, such as HIV and hepatitis. Also, injected vaccines need trained personnel and mass vaccinations are cumbersome as it takes a long time to immunize large groups of people.
“In light of the risk of serious, worldwide infections, so-called pandemics, we want to be able to mass vaccinate people against fast spreading infections such as influenza or Ebola. This is why spray and drinkable vaccines, in particular, are very attractive,” explains Professor Nils Lycke.
A vaccination is intended to stimulate our immune system to specifically protect against infections caused by bacteria, viruses or parasites. Upon vaccination, an antigen unique to the infection is administered, this is usually a protein or proteins unique to the disease-causing microorganism. The desirable result from vaccination is that the immune system forms protective antibodies and expands also the cell-mediated adaptive immune response that protects us against infection.
“We are working on non-living vaccines. These need to be given together with an immune-enhancing substance, i.e. an adjuvant, which is a critical component to evoke a sufficiently strong immune response. Today, live viruses, attenuated and weakened, are also used for vaccinations, but such vaccines are more difficult to handle and are less stable than ’killed’ vaccines. They give a mild pathogenic effect. An example of such a vaccine is the measles virus vaccine.”
Mucosal vaccines
An efficient and safe way of mass vaccination would be to give the vaccine in the form of a nasal spray or as a drinkable vaccine. Such vaccines activate the immune system via the mucous membranes in the respiratory passages or in the gastrointestinal canal. An advantage of mucosal immunizations is that the risk of side effects is significantly lower compared with injectable vaccines.
“Most infections that affect us are caused by microorganisms that enter the body via our mucous membranes, so a strong local immune response at the mucosal membranes is highly protective and a very attractive feature in the next generation of vaccines.”
Today, there are only a handful of mucosal vaccines, for example there is a nasal spray against influenza and a drinkable vaccine against Rota virus or cholera. A reason for the poor number of killed mucosal vaccines is that these usually require large amounts of antigen and a strong and safe adjuvant. It has to be remembered that most of what is given orally is digested and degraded by enzymes that are found in the gastrointestinal canal. Therefore, it is expensive and difficult to make effective mucosal vaccines based on proteins.
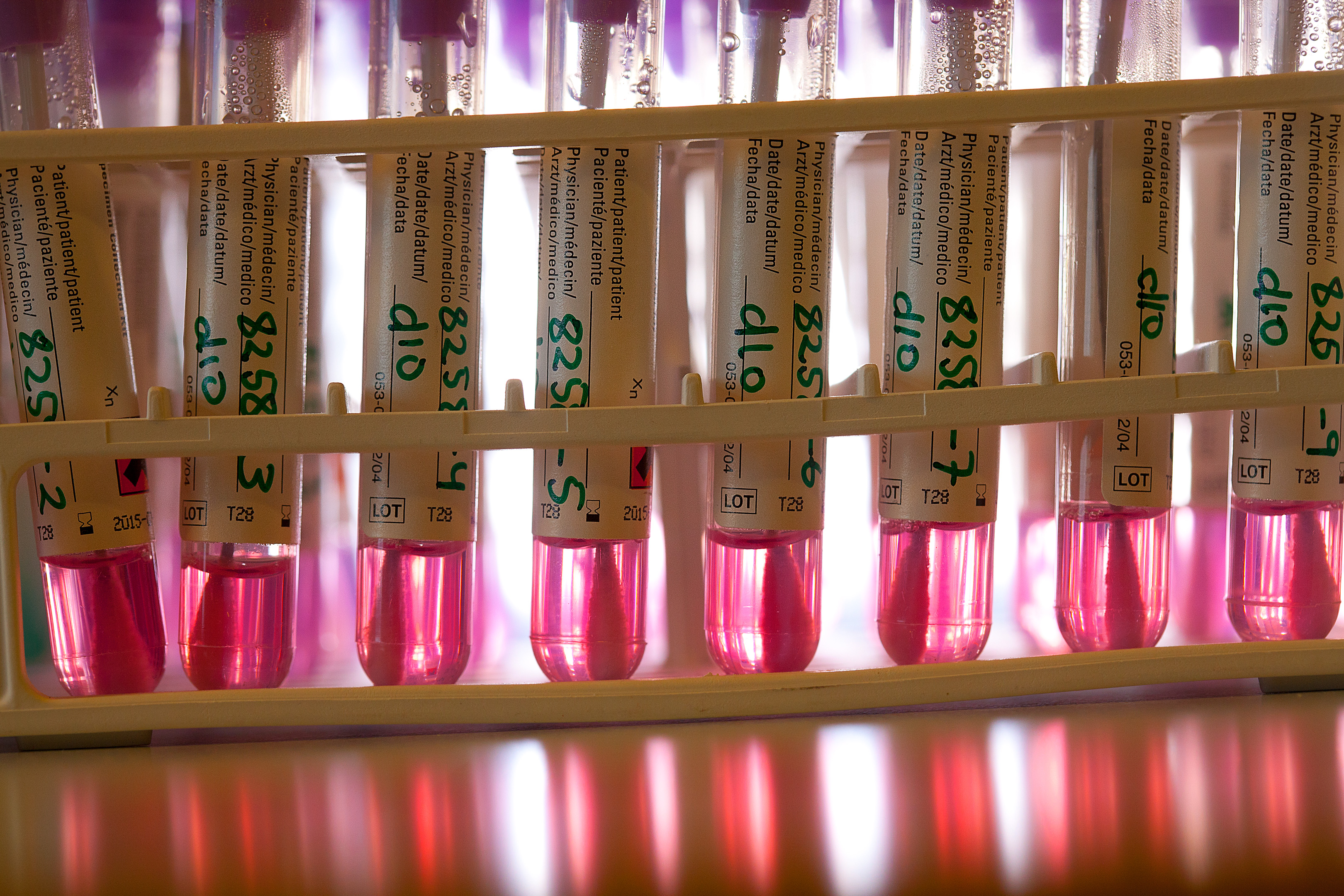
The goal of our project is, therefore, to circumvent the problem of stability and degradation by developing a more robust and efficient immunoenhancing vaccine using a patented adjuvant CTA1-DD. Hereby, we succeed in sparing antigen dose as well as we will augment the vaccine stimulation ability of a strong immune response. Also, by “packaging” the vaccine in a new way in nanoparticles, we will allow more antigen to be taken up by the mucosal immune system. “This is how we envisage that the next generation of drinkable and spray vaccines will prove mucosal vaccination realistic and a competitive alternative to today’s injectable vaccines.”
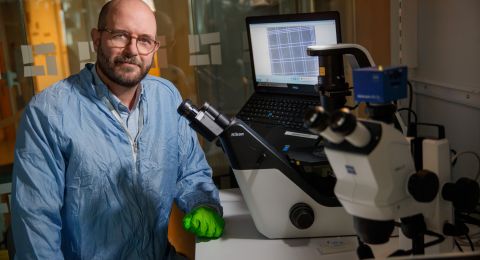
A general and effective module
The packaging is, therefore, a way to combine the nanoparticle with an effective adjuvant in an effective module that can function as a carrier of many different vaccines against many types of pathogens. The ambition is also to target the particles to specific cells of the immune system that are known to initiate an immune response. These are dendritic cells in the mucosal membranes of the respiratory tract or the gastrointestinal canal. The strategy to target the dendritic cells will employ antibodies directed against surface molecules on these cells. The antibodies will be expressed as part of the adjuvant as a single protein molecule with the CTA1-moiety. The dendritic cells are the body’s most important cells to take up foreign antigens and to stimulate immune responses.
“The nanoparticles in our project will be made of fat, lipids, and perhaps some sugar structures, will be tested, to protect and target our vaccine antigens to the mucosal immune system. The nanoparticles will protect against degradation by enzymes in the gastrointestinal canal. The particles should also be designed so that they find their way through the mucous and can be effectively taken up by the dendritic cells in the mucosal membrane.”
The adjuvant that the project has developed is a so-called fusion protein, CTA1-DD and it consists of an active enzyme, CTA1, from the cholera toxin produced by Vibrio cholera bacteria. The fusion protein can also host a vaccine component and as discussed a targeting unit to directly bind to dendritic cells in the mucosal membrane. The fusion protein strategy will allow small amounts of antigen to effectively stimulate an immune response.
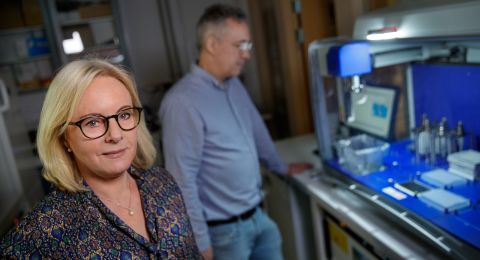
Complementing expertise
The project is a high-risk project. The researchers are nonetheless optimistic, in part because they work across disciplines with complementary expertise. Researchers in immunology, nanobiotechnology, glycobiology, virology, and vaccine development are involved in the project.
“This project is wonderful and fantastic in that it allows us to develop a completely new vaccine concept. It is always stimulating to try to do something no one before you have achieved and to succeed in developing next generation of effective mucosal vaccines. Working this way is exciting because it creates interesting breakpoints between different scientific disciplines and expertise.”
The project may also provide important new knowledge on how to vaccinate against autoimmune diseases, such as type 1 diabetes, Multiple sclerosis or rheumatoid arthritis.
Text Anders Esselin
Translation Semantix
Photo Magnus Bergström